Research

Research Grants
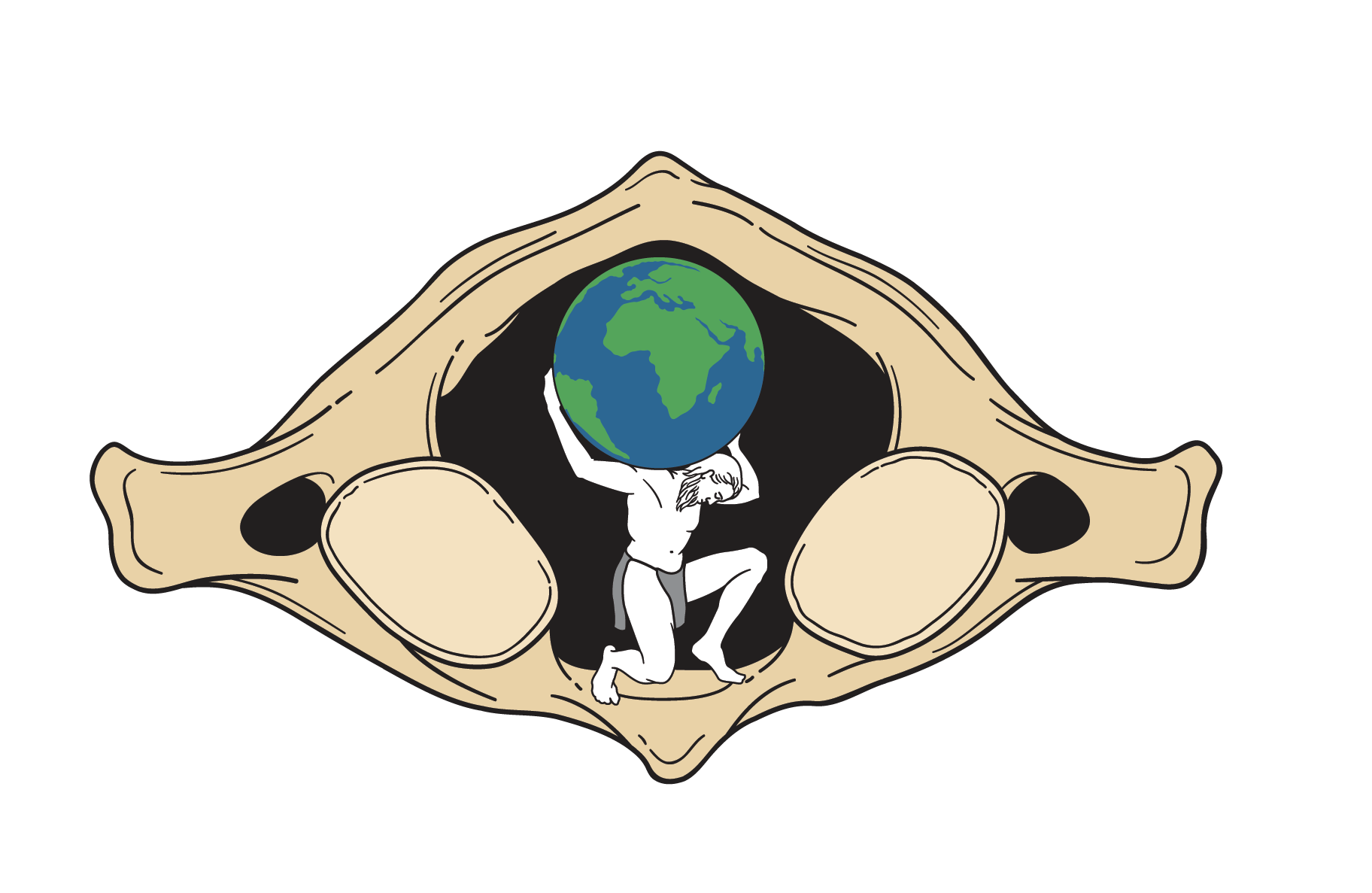
The mission of the Cervical Spine Research Society is to carry out research and exchange information on the cervical spine.

Research Paper Award Information
The mission of the Cervical Spine Research Society is to carry out research and exchange information on the cervical spine. To help achieve this goal, the Society is offering awards for outstanding, unpublished research papers.